Bone & Joint Health, Exercise & Injury Prevention, Joint Knowledge
Joint Knowledge: The Ankle
The ankle is a hinge joint made up of three bones: the tibia (shinbone) and fibula (the lateral bone of the leg), and the talus (foot bone). They two bones on the lower leg join with the talus to form the ankle joint.
In addition to the tibia, fibula, and talus, proper function of the ankle involves ligaments, cartilage, tendons, muscles, and nerves, too. This complexity makes the ankle incredibly versatile. However, it also makes it prone to injury. Here’s what you need to know to keep your ankles healthy.
How the Ankle Moves
The talus also connects to the calcaneus (aka, the heel bone). A healthy ankle allows the foot to move up, down, and side to side.
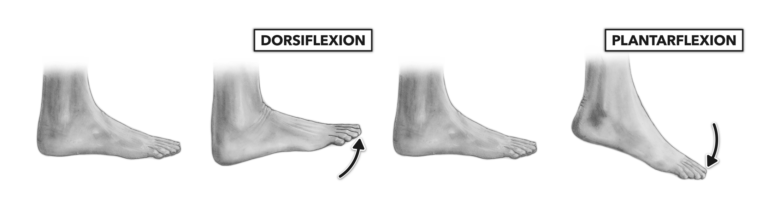
These specific ankle movements are called: dorsiflexion, plantarflexion, inversion, and eversion.

Ligaments help stabilize the ankle during these movements, preventing excessive inversion and eversion. Five ligaments sit on the inner side of the ankle (also known as the medial aspect of the ankle), and three sit on the outer side (or, the lateral aspect of the ankle).
The lower leg muscles power the movement of the ankle. Ankle dorsiflexors and toe extensors reside in the anterior (front) lower leg. These include the tibialis anterior, extensor digitorum longus, extensor hallucis longus, and peroneus tertius.
The peroneal muscles reside in the lateral (side) lower leg. These enable plantar (the sole of the foot) flexion and eversion.
Also vital for plantar flexion and toe flexion are the muscles of the posterior (back) lower leg. These include the gastrocnemius, soleus, tibialis posterior, flexor digitorum longus, and flexor hallucis longus.
Phew! Who knew the ankle was so complex??
Ankle Injuries
Lateral ankle sprains (LASs) are one of the most common sports injuries, with roughly 23,000 instances occurring every day in the United States!
Each year, 1.5 to 2 million U.S. residents experience a LAS, with annual health care costs related to LASs adding up to about $4.2 billion. These costs include approximately 1.6 million physician visits, 600,000 emergency room visits, and 8,000 hospitalizations each year.
Yet, these numbers only account for treatment. Many LASs result in long-term discomfort, limited mobility, and post-traumatic swelling of the ankle. These outcomes often significantly limit physical activity, thus increasing the risk of obesity and associated health issues.
About 30 to 70 percent of people who experience a LAS go on to develop chronic ankle instability (CAI). People with CAI experience persistent discomfort, perceived instability, and recurring sprains or other forms of ankle failure for at least 12 months after the LAS.
Many ankle injuries cause long-term deformities in the joint and/or the surrounding cartilage and bone. This alters the way the ankle moves, often limiting certain ranges of motion and causing weakness.
Preventing Ankle Injuries
Ankle sprains occur when the ankle exceeds its normal range of motion. As mentioned above, the most common type of sprain in is the lateral ankle sprain: the ankle moves too far into inversion (take a peek at the inversion image above!), spraining the lateral ligaments of the ankle.
The supporting ligaments stretch and tear, resulting in a sprain. The greater the tear, the more serious the sprain. Ankle sprains are common in sports such as soccer, football, rugby, tennis, and others that demand lots of running and quick changes in direction. Elderly people and people with preexisting joint issues are also more prone to ankle sprains.
While proper medical care can significantly improve the prognosis following an ankle sprain, prevention is always preferred. You can minimize your risk of a LAS and other types of ankle injuries by improving your strength, flexibility, and balance.
Strengthening Exercises
It’s important to strengthen the muscles of the legs, particularly the shins and calves. This reduces the force your ankles have to bear during movements such as running and jumping. In this regard, it is equally important to build strength in the hips, core, and back.
You can achieve this through exercises like crunches, sit-ups, squats, and deadlifts. Your doctor or physical therapist can help you develop a safe and effective exercise regimen.
Flexibility
Stretch and warm-up before engaging in physical activity. Warm-up with a light activity that mimics the movements you will be performing. Next, perform simple stretches such as toe touches, calf stretches, and ankle flexion, extension, and rotation.
Perform these stretches with light to moderate intensity, as stretching too hard can inhibit muscle performance.
A Balancing Act
Balance is a combination of three systems. What you see gives your body a basic blueprint for how to move. The nerves throughout your body refine this information via proprioception. Your nerves allow you to sense pressure, impact, and other forces you encounter. The last component of balance is your vestibular system, powered by your inner ear. This lets you know your position within your environment, whether you’re running, spinning, upside-down, falling, etc.
You can improve your balance, particularly as it relates to ankle stability by performing one-legged exercises. For example, you can stand on one leg for time, or perform dynamic exercises like single-leg hops and step-ups. The muscles and nerves in your body will adapt to these movements and become better equipped to stabilize you during intense exercise.
Proper physical conditioning can help you avoid ankle sprains. In the event of an ankle sprain, seek immediate medical care, and follow your doctor’s advice to facilitate proper healing and minimize complications.

